This article provides an overview of interstitial cystitis, including how it is different from a urinary tract infection (UTI). It also covers treatment options, including at-home care for bladder pain syndrome.
How common is interstitial cystitis?

Statistics about the prevalence of interstitial cystitis vary. The American Urological Association (AUA) notes that the lack of a standard method for diagnosing interstitial cystitis makes it difficult to accurately estimate the number of people who have it.
The National Kidney Foundation (NKF) reports that about 700,000 to 1 million people in the United States have interstitial cystitis. The AUA estimates that up to 12 million people experience symptoms of interstitial cystitis. They add that women are more likely to have the condition, with up to 8 million women experiencing symptoms compared with up to 4 million men.
Interstitial cystitis vs. urinary tract infection
The symptoms of interstitial cystitis are very similar to those of a UTI. These include pain near the bladder, discomfort when urinating, and a frequent need to go to the bathroom.
However, each condition has different causes and treatments. A UTI results from bacteria that enter the bladder. Taking antibiotics treats the infection and helps symptoms subside.
With interstitial cystitis, no infection is present, and the symptoms have no clear cause. As a result, treatment focuses on managing and minimizing symptoms.
Symptoms of interstitial cystitis
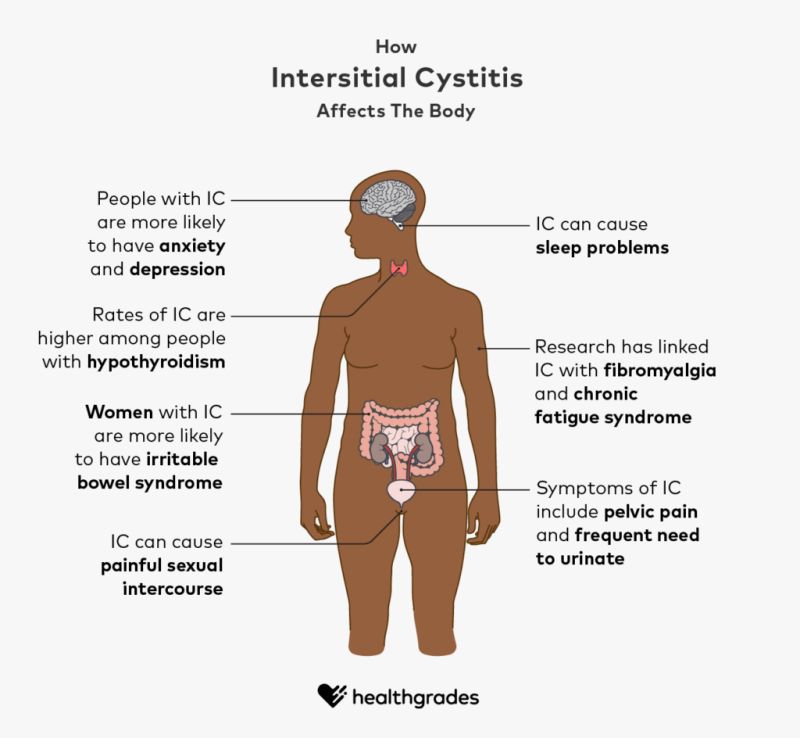
Symptoms of interstitial cystitis include pelvic pain, pressure, or discomfort and the need to urinate urgently or frequently. Blood may occasionally be present in the urine. Over time, the bladder may not be able to hold as much urine.
Common symptoms of interstitial cystitis
Symptoms of interstitial cystitis vary. If you have interstitial cystitis, you may experience some or all of these symptoms:
- difficult or painful urination, or burning with urination (dysuria)
- an urgent need to urinate
- frequent urination that often produces only a small amount of urine
- bloody or pink urine (hematuria)
- pain during sexual intercourse
- pelvic pain, pressure, or discomfort
- sleep disturbance
Serious symptoms that might indicate a life threatening condition
In some cases, symptoms of interstitial cystitis can accompany a serious or potentially life threatening condition. Seek immediate medical care (call 911) for any of these life threatening symptoms:
- high fever (higher than 101ºF or 38ºC)
- an inability to urinate
- severe pelvic pain
Seek prompt medical care if you have such symptoms as pelvic pain, pressure, or discomfort or you need to go to the bathroom frequently or urgently. If you are currently receiving treatment for interstitial cystitis, talk with your doctor if your symptoms do not improve or they go away and come back.
What causes interstitial cystitis?
The specific cause of interstitial cystitis is not known. The Interstitial Cystitis Association (ICA) explains that researchers think that certain triggers may cause damage to bladder tissue that can lead to the development of interstitial cystitis.
The ICA lists these possible triggers:
- trauma to the bladder, such as from pelvic surgery
- pelvic floor muscle problems
- an autoimmune condition
- a bacterial infection, such as cystitis
- inflammation of the nerves in the pelvic area
- spinal cord trauma
- overdistention of the bladder from long periods without going to the bathroom
The AUA notes that some researchers believe that damage to the lining of the bladder allows substances from urine to penetrate and irritate the bladder wall.
Research suggests that up to
Risk factors for interstitial cystitis
According to the AUA, experts have not identified any specific habits or behaviors that increase your risk of developing interstitial cystitis. However, they add that certain people may have a substance in their urine that makes their bladder tissue more vulnerable to
interstitial cystitis.
Research in the
- depression
- chronic pain
- inflammatory conditions
- mood disorders
- anxiety
- hypothyroidism
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) reports that women with interstitial cystitis are also more likely to have:
- fibromyalgia
- chronic fatigue syndrome
- irritable bowel syndrome
The NIDDK goes on to say that people with interstitial cystitis may also be more likely to have allergies and certain autoimmune conditions.
If you have risk factors, talk with your primary care doctor or urologist about any concerns you have about developing interstitial cystitis or if you develop symptoms.
Diet and nutrition tips for interstitial cystitis
Experts suggest that certain foods can help you manage or minimize interstitial cystitis symptoms, while others can trigger flares.
To identify the foods that may worsen or improve your symptoms, it may be helpful to keep a food diary for a few weeks. You may also want to work with your doctor to try an elimination diet, where you remove certain foods then slowly add them back to your diet to see which ones worsen your condition.
Foods to help manage interstitial cystitis symptoms
The AUA lists these interstitial cystitis-friendly foods:
- fruits including bananas, honeydew melons, blueberries, and apples
- vegetables including green beans, black-eyed peas, bell peppers, celery, and asparagus
- dairy products including cheese, milk, and certain types of sherbet
- beverages including water, non-soy milk, chamomile or peppermint tea, and pear or blueberry juice
Foods to avoid with interstitial cystitis
The AUA recommends staying away from these foods:
- acidic fruits including oranges, grapefruit, lemon, lime, and pineapple
- vegetables including tomato and tomato products, pickles, sauerkraut, onions, and chili peppers
- dairy products including items with chocolate, soy products, processed cheeses, and yogurts flavored with chocolate, lemon, lime, or orange
- beverages including alcohol, coffee, sports drinks, cranberry juice, chocolate drinks, and herbal or green teas
Talk with your primary care doctor or urologist before making any significant changes to your diet. They may refer you to a nutritionist or dietitian who can provide guidance on healthy food choices with interstitial cystitis.
How doctors diagnose interstitial cystitis
To diagnose interstitial cystitis, your doctor or licensed healthcare practitioner will perform a physical exam, take your medical history, and possibly perform a series of tests.
To evaluate your symptoms, they may ask you questions such as:
- What are your symptoms?
- When did your symptoms start?
- Does anything make your symptoms go away or worsen?
- Do you frequently feel the need to urinate? Does the urge to urinate come on suddenly?
- When you urinate, is the urine clear or cloudy?
- Are you having pain during sexual intercourse?
- Do you have frequent UTIs?
- Do you have any other medical conditions?
- Are you taking any medications, including antibiotics?
Testing for interstitial cystitis
There is no specific test to diagnose interstitial cystitis. Because its symptoms overlap with those of several other conditions, your doctor will first need to rule out other possible causes.
Tests your doctor may order or perform include:
- Urinalysis: This test helps your doctor rule out an infection.
- Cystoscopy: In this procedure, a doctor inserts a long, narrow tube with a camera, called a cystoscope, into the urethra and up to the bladder. This allows the doctor to view the inside of the bladder for ulcers, bleeding, or signs of cancer.
- Bladder distention or instillation: As part of a cystoscopy procedure, the doctor may slowly fill your bladder with liquid to test how much urine it can hold.
- Biopsy: During a cystoscopy procedure, your doctor may also remove a sample of tissue from your bladder to test for cancer.
Treatments for interstitial cystitis
There is currently no cure for interstitial cystitis, but treatment options are available to help minimize and manage symptoms.
Guidelines in the European Medical Journal outline a progression of treatment for people with non-ulcerative interstitial cystitis, starting with lifestyle changes and at-home care.
Non-medical treatments for interstitial cystitis
Lifestyle habits and therapies to help manage interstitial cystitis symptoms include:
- making changes to your diet to eliminate food triggers
- trying bladder training, including urge suppression and distraction techniques
- reducing stress, such as through yoga, exercise, or massage
Medications for interstitial cystitis
If at-home treatments are not effective, your doctor may recommend or prescribe medications including:
- pentosan polysulfate, which is the
only oral medication Trusted Source PubMed Central Highly respected database from the National Institutes of Health Go to source with Food and Drug Administration (FDA) approval for the treatment of interstitial cystitis - antihistamines, such as hydroxyzine (Vistaril), to reduce urinary frequency
- non-narcotic pain relievers, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), or indomethacin (Indocin)
- tricyclic antidepressants, such as amitriptyline (Elavil), for the relief of pain and urinary frequency
Bladder dilation for interstitial cystitis
The same distention procedure that doctors may use to diagnose interstitial cystitis can also be an effective treatment option for the condition in some people.
During bladder dilation, a doctor slowly fills the bladder with sterile water to stretch and expand the bladder wall.
Intravesical therapy for interstitial cystitis
Similar to bladder dilation, intravesical therapy is a procedure in which a doctor slowly fills the bladder with a medicated liquid to apply a medication directly to the bladder wall. Another name for this procedure is bladder instillation.
The NKF lists these types of bladder instillations:
- dimethyl sulfoxide, which reduces inflammation and pain
- heparin
- Bacille Calmette-Guérin, which is a treatment currently in clinical trials
- hyaluronic acid (Cystistat), which is another experimental treatment currently in clinical trials
- bladder “cocktails,” which are combinations of several medications into one mixture
Nerve stimulation for interstitial cystitis
The NKF describes two types of electronic nerve stimulation to help relieve pain and other symptoms of interstitial cystitis. Those are transcutaneous electrical nerve stimulation (TENS) and
sacral nerve stimulation implants.
TENS uses an external device to deliver electrical pulses to relieve pain, while sacral nerve stimulation implants use a device that has FDA approval for treating urinary incontinence and that is currently undergoing tests as a treatment for interstitial cystitis.
Surgery for interstitial cystitis
When other treatment options are not effective, a doctor may consider bladder surgery to treat interstitial colitis. Surgery for interstitial cystitis is not reversible and can cause several complications.
The ICA lists the following surgical treatments for the condition:
- urinary diversion, which is a procedure that redirects urine around the bladder and through a surgically created opening in the abdomen
- orthotopic diversion, which is a procedure that removes the bladder and replaces it with a new bladder constructed from bowel tissue
- augmentation cystoplasty, which is a procedure that removes some or most of the bladder and reconstructs it with bowel tissue
For people who have interstitial cystitis with areas of scarring known as Hunner’s lesions, a doctor may recommend laser surgery as a first-line treatment.
Your urologist will discuss all of your treatment options in the context of your individual diagnosis so that you can work together on a treatment plan that is right for you.
Potential complications of interstitial cystitis
Complications of untreated interstitial cystitis can be serious. You can help minimize your risk of serious complications by following the treatment plan that you and your healthcare professional design specifically for you.
Some possible complications of interstitial cystitis include:
- decreased bladder capacity
- kidney damage due to long-term high bladder pressure
- permanent or chronic pain
Summary
Interstitial cystitis causes pain and several other symptoms in the urinary tract and pelvic area. Specifically, you might experience a sensation of pelvic pressure, pain during sexual intercourse, and an urgent need to urinate.
There are plenty of treatment options available for interstitial cystitis. Discuss with your doctor the best treatment option for you.



















